What Does Female Infertility mean?
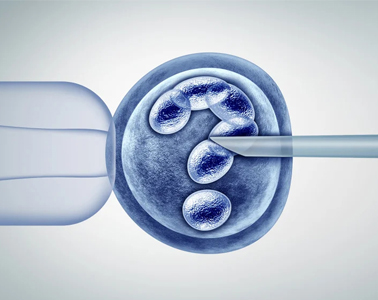
Infertility is generally understood to be the inability to conceive after one year (or more) of unprotected intercourse. Some healthcare professionals assess and treat women aged 35 or older after six months of unprotected intercourse because it is known that women's fertility declines progressively with age.